Chronic Kidney Disease (CKD) is a growing global health concern, especially among high-risk populations such as individuals with diabetes, hypertension, or a family history of kidney disorders. Early detection and proactive management are crucial to slowing disease progression and improving quality of life.
1. Early Screening and Diagnosis of CKD
Who Is at Risk?
Routine CKD screening is recommended for:
-
Diabetic patients
-
Individuals with high blood pressure
-
Obese individuals
-
Those with a family history of kidney disease
-
Patients regularly using NSAIDs or exposed to nephrotoxic substances
Diagnostic Methods
-
Annual blood tests: Measuring serum creatinine to calculate the estimated Glomerular Filtration Rate (eGFR) using the CKD-EPI formula.
-
Urine analysis: Albumin-to-creatinine ratio (ACR) for detecting proteinuria.
Diagnosis Confirmation: Persistent abnormalities for over 3 months such as:
-
eGFR < 60 mL/min/1.73 m²
-
Presence of albuminuria, hematuria, or kidney structural anomalies
2. Initial Assessment and Risk Stratification
Identifying the Cause
-
Evaluation for diabetes, hypertension, glomerulonephritis, or polycystic kidney disease.
Risk Categorization
-
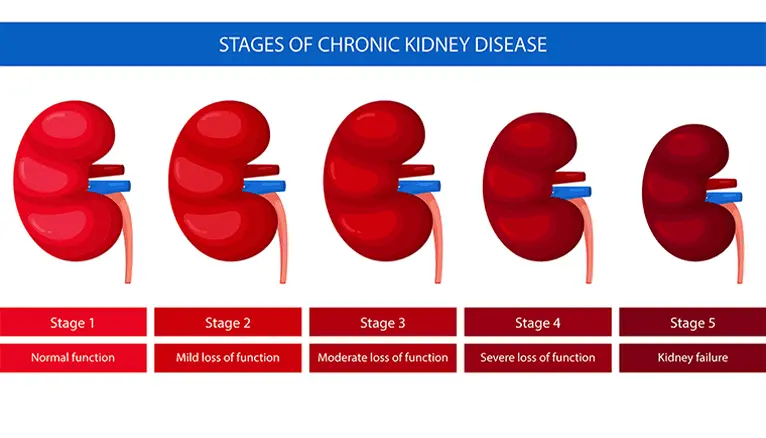
CKD staging: Based on eGFR levels (Stages 1 to 5).
-
Albuminuria grading: Categories A1 to A3.
-
Kidney Failure Risk Equation (KFRE):
-
≥3% risk in 5 years → Referral to a nephrologist
-
≥10% risk in 2 years → Multidisciplinary care recommended
-
3. Kidney-Protective Treatment Plan
Lifestyle and Dietary Changes
-
Low-protein diet: 0.6–0.8 g/kg/day
-
Sodium restriction: 4–6 g/day
-
Potassium control: Especially in cases of hyperkalemia
-
Hydration management: Based on fluid volume status
-
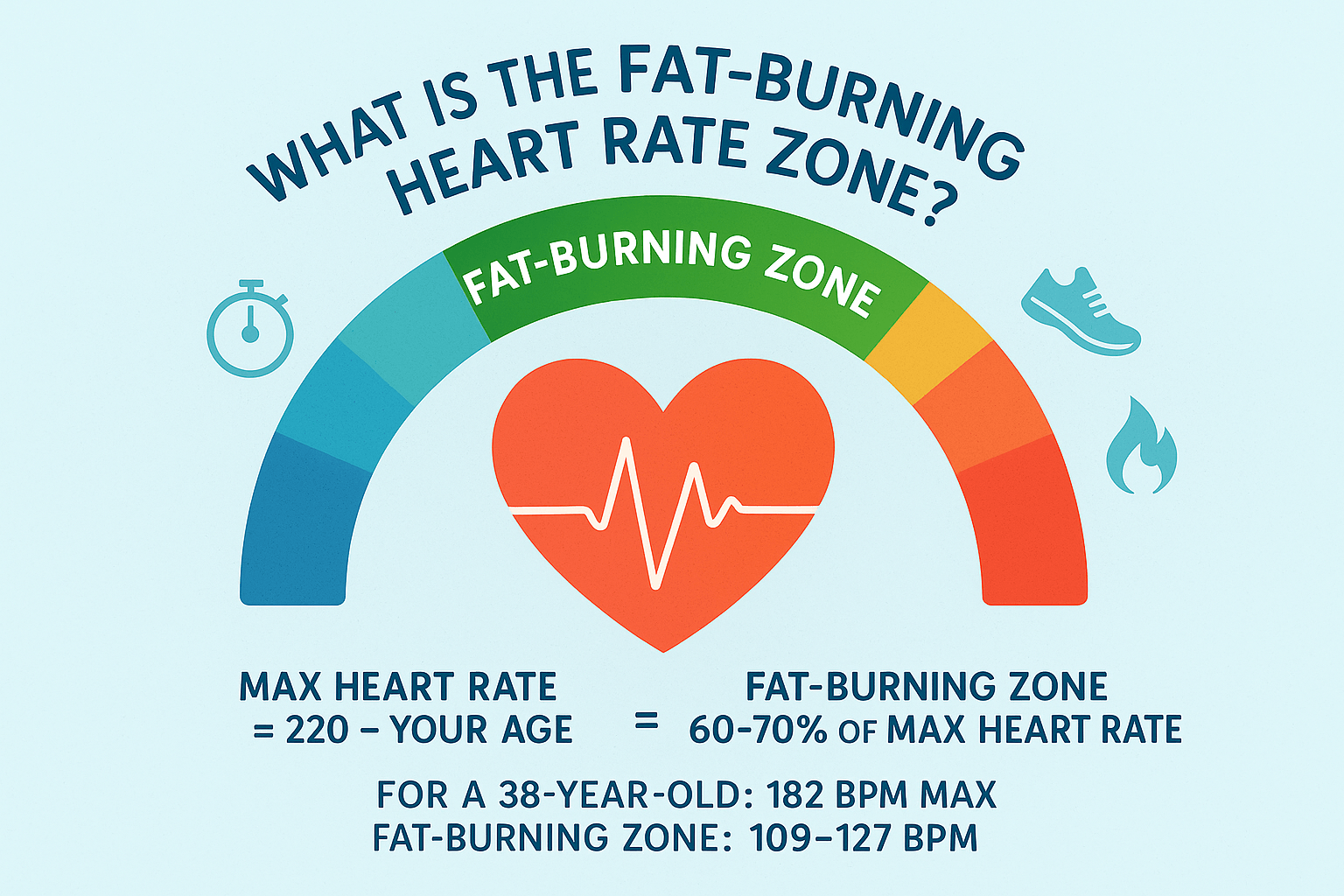
Smoking cessation and regular physical activity
Blood Pressure Control
-
Target BP:
-
<130/80 mmHg if ACR > 300 mg/g
-
<140/90 mmHg otherwise
-
-
Preferred medications:
-
ACE inhibitors (ACEIs) or angiotensin receptor blockers (ARBs)
-
Diuretics (thiazide or loop like furosemide)
-
Consider spironolactone or chlorthalidone if blood pressure remains high
-
Specific Therapies
-
SGLT2 inhibitors (e.g., dapagliflozin): Delay CKD progression and reduce cardiovascular risks
-
GLP-1 receptor agonists (e.g., semaglutide)
-
Treating anemia: Iron supplementation and erythropoietin
-
Correcting metabolic acidosis: Sodium bicarbonate therapy
4. Ongoing Monitoring and Follow-Up
Check-Up Frequency
-
CKD Stages 1–2: Annual testing of eGFR and ACR
-
CKD Stages 3A–5: Monitoring every 3–6 months depending on progression
Comorbidity Management
-
Cardiovascular risk reduction: LDL cholesterol target < 0.55 g/L in high-risk patients
-
Screening for heart failure and metabolic imbalances (e.g., hyperphosphatemia, hypocalcemia)
5. Referral to a Nephrologist
When to Refer
-
eGFR < 45 mL/min (or < 20 mL/min in older adults)
-
Rapid decline in kidney function (>2 mL/min/year)
-
Severe albuminuria (ACR > 500 mg/g)
-
Uncontrolled hypertension despite treatment
Planning for Kidney Replacement Therapy
-
Early education on dialysis, kidney transplant, and conservative care options starting at CKD Stage 4
-
Shared decision-making with the patient
6. Latest Advances and Preventive Measures
New Treatments
-
Non-steroidal mineralocorticoid receptor antagonists (e.g., finerenone)
-
Difelikefalin for managing uremic pruritus
Recommended Vaccinations
-
Influenza
-
COVID-19
-
Hepatitis B
-
Pneumococcal infections