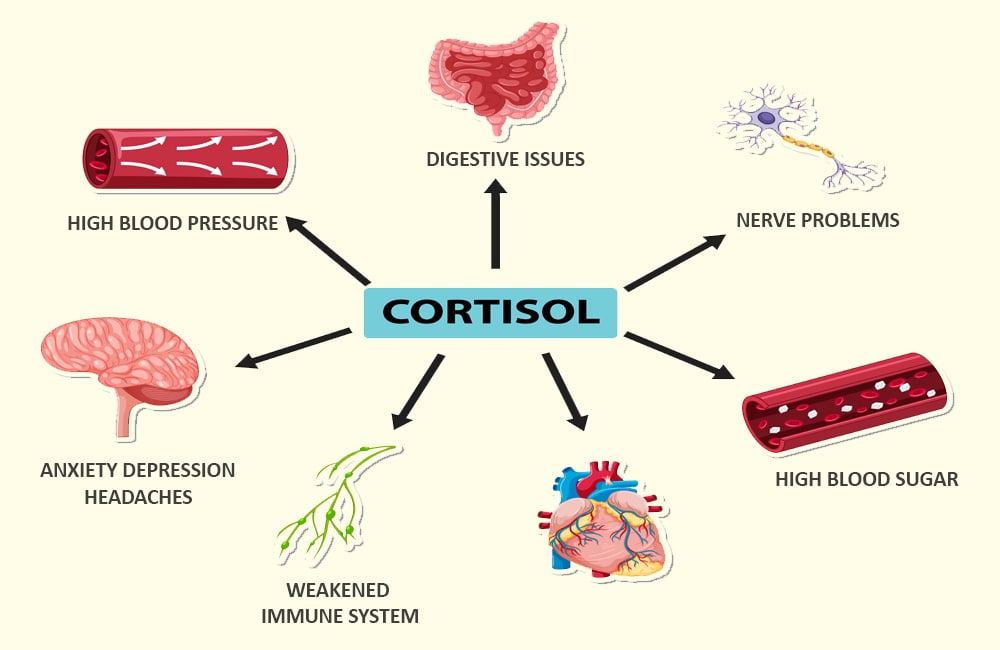
Cortisol, often referred to as the “stress hormone,” plays an essential role in the body’s natural stress response, metabolism, and immune regulation. When levels of cortisol remain elevated for extended periods, they can contribute to a host of physical and emotional problems. In this detailed exploration, we delve into the nature of cortisol, the underlying causes of its elevated production, and the various symptoms that may signify an imbalance. By drawing on the expertise reflected in health articles from reputable sources, we provide a comprehensive guide designed to foster public health awareness and educate readers on how to manage and reduce high cortisol levels.
Understanding Cortisol: Its Functions and Role in the Body
Cortisol is produced in the adrenal glands and is instrumental in managing the body’s response to stress. In normal doses, this hormone regulates metabolism, aids in memory formation, helps control blood sugar levels, and reduces inflammation. However, in the face of chronic stress or underlying medical issues, the body may produce too much cortisol, leading to adverse consequences.
In times of acute stress, cortisol helps the body mobilize energy resources quickly, a survival mechanism dating back to early human evolution. This so-called “fight-or-flight” response prepares the body to react to immediate dangers. Once the perceived threat subsides, cortisol levels naturally decrease. However, when stress persists over long durations—whether due to personal, professional, or environmental factors—this finely tuned system can become unbalanced. Over time, persistently elevated cortisol levels can disrupt many bodily processes, affecting everything from weight regulation to cognitive functions.
Recent studies have underscored cortisol’s role in the interplay between physical and mental health. Researchers have found that chronic cortisol elevation may result in symptoms ranging from fatigue and weight gain to impaired concentration and mood disturbances. These findings highlight the necessity of managing stress and monitoring cortisol levels as integral components of preventive healthcare.
The intricacy of cortisol’s role in the body underscores its importance. Being fully aware of how this hormone functions helps us understand why managing stress and maintaining a healthy lifestyle are essential for overall well-being.
The Physiology Behind Cortisol Regulation
To appreciate why cortisol levels can rise and the ensuing effects on health, one must first understand its production and regulation. Cortisol synthesis follows a complex pathway known as the hypothalamic-pituitary-adrenal (HPA) axis. This system orchestrates the release of cortisol into the bloodstream and ensures that its levels are maintained within an optimal range.
In brief, the process begins in the hypothalamus when the brain perceives stress. The hypothalamus signals the pituitary gland, which then releases adrenocorticotropic hormone (ACTH). ACTH stimulates the adrenal glands, prompting the production of cortisol. Under normal circumstances, negative feedback mechanisms signal the brain to reduce the production of ACTH once cortisol has reached sufficient levels. However, when the stress response is constantly activated, these feedback loops may falter, leading to consistently high cortisol levels.
This delicate balance between activation and inhibition of the HPA axis is essential to prevent the negative health effects associated with prolonged cortisol elevation. An imbalance in this system has been linked to various metabolic, cardiovascular, and mental health disorders. Such dysregulation explains why conditions such as Cushing’s syndrome—a disorder characterized by abnormally high cortisol levels—present with multiple systemic manifestations.
Understanding these physiological processes is critical for both healthcare professionals and the general public. When discussing cortisol-related disorders, it is important to note that the hormone itself is not harmful. Instead, it is the chronic elevation stemming from misregulated body systems and persistent stress that leads to problematic outcomes.
Triggers of Elevated Cortisol Levels
The causes of elevated cortisol levels are multifaceted, ranging from external stressors to internal health conditions. Recognizing the triggers is the first step toward prevention and effective management.
Chronic Stress and Lifestyle Factors
One of the most common drivers of heightened cortisol is chronic stress. In modern society, stressors abound—from job pressures and financial worries to family conflicts and societal uncertainties. Persistent psychological stress continuously stimulates the HPA axis, preventing cortisol from ever settling at a healthy baseline. Over time, this chronic activation can lead to a range of health issues.
Sleep deprivation is a frequent companion to stress. Poor sleep quality not only acts as a stressor in itself but also impairs the body’s ability to regulate hormones correctly. Individuals who experience ongoing sleep disturbances often find that their cortisol levels remain higher than normal, even during periods intended for rest and recovery.
Moreover, dietary habits and lack of physical exercise can exacerbate the body’s stress response. High intake of processed foods, excessive caffeine, and alcohol consumption can overload the system, making it harder for the body to regulate hormonal responses effectively. Incorporating mindful eating practices and regular physical activity is essential in mitigating these effects.
Medical Conditions and Medications
Certain underlying medical conditions can also lead to elevated cortisol. For example, adrenal gland disorders, including adrenal hyperplasia and tumors, may cause the overproduction of cortisol. Additionally, disorders such as Cushing’s syndrome are directly linked to abnormal cortisol secretion. While Cushing’s syndrome is relatively rare, its clinical manifestations underscore the profound effects of cortisol dysregulation on the body.
Some medications, particularly those used in chronic inflammatory diseases, may interfere with cortisol production. Corticosteroid drugs, when used over long periods, mimic the actions of cortisol in the body. Although these medications are invaluable in treating conditions like rheumatoid arthritis and asthma, their prolonged use can contribute to a state of cortisol excess if not carefully managed by a healthcare professional.
Psychological Disorders and Long-Term Anxiety
Anxiety and depression can also be significant contributors. Research has shown that individuals suffering from these conditions tend to exhibit higher baseline levels of cortisol. This interrelationship is complex; while elevated cortisol can worsen mood disorders, the constant mental strain from anxiety can further exacerbate hormonal imbalances. This cyclical dynamic makes addressing mental health an integral part of managing cortisol levels.
Understanding these triggers reveals that the road to achieving healthy cortisol levels is not solely about mitigating stress in one’s personal life. It also involves managing sleep, nutrition, and any underlying medical or psychological conditions. This comprehensive approach underscores how interconnected our bodily systems are, and why addressing cortisol dysregulation requires both lifestyle adjustments and, in some cases, clinical intervention.
Recognizing the Warning Signs of High Cortisol
The human body often communicates subtle signals when something is amiss. Elevated cortisol levels can produce a range of symptoms, many of which overlap with other conditions, making early detection challenging but crucial for effective treatment.
Physical Manifestations
Chronic high cortisol is frequently associated with weight gain, particularly in the abdominal area. This specific fat distribution, often termed “central obesity,” is due to cortisol’s role in fat metabolism. Alongside weight gain, patients often experience thinning skin, which may bruise more easily, and muscle weakness—a result of cortisol’s catabolic effects on muscle tissue.
Another common physical complaint is high blood pressure. Prolonged exposure to elevated cortisol can lead to increased blood volume and vascular resistance, raising the risk for hypertension and other cardiovascular issues. Some patients also report changes in their skin, such as stretch marks, which are indicative of rapid changes in body composition.
Fatigue and low energy levels, despite adequate sleep, can also signal excess cortisol. The body’s inability to shift into a recuperative state due to constant hormone production can lead to an overwhelming sense of tiredness. Additionally, frequent headaches, gastrointestinal disturbances, and even irregular menstrual cycles in women have been noted in individuals with persistently high cortisol levels.
Cognitive and Emotional Symptoms
In addition to physical symptoms, high cortisol can have significant impacts on mental health and cognitive function. Individuals may experience mood swings, irritability, and a general sense of anxiety. Over time, these mood changes can evolve into more persistent conditions such as depression or generalized anxiety disorders.
Memory lapses and difficulty concentrating are also reported, suggesting that elevated cortisol may affect brain regions responsible for learning and memory, such as the hippocampus. This cognitive decline can have serious ramifications for both professional performance and personal quality of life.
Sleep disturbances are another important sign. Many individuals with high cortisol find themselves caught in a vicious cycle where stress leads to sleep problems, which in turn fuel further cortisol production. This endless loop not only hampers daily functioning but also exacerbates overall stress levels.
Subtle and Overlooked Indications
Some of the more subtle signs of high cortisol can go unnoticed until they become more pronounced. For example, in many cases, the initial symptoms such as slight weight gain, intermittent fatigue, or occasional anxiety may be dismissed as typical responses to everyday stress. However, if these symptoms persist and progressively worsen, they may indicate a more systemic issue.
It is important to adopt a holistic view of health—if multiple symptoms are present, it might be wise to consult a healthcare provider for a more comprehensive assessment. Recognizing these early signs can lead to timely interventions that prevent more serious health complications from developing.
The Complex Relationship Between Cortisol and Mental Health
The connection between elevated cortisol and mental health is a subject of extensive research and clinical discussion. The brain, being one of the primary targets of cortisol, is highly susceptible to the effects of chronic hormone imbalance.
Stress, Anxiety, and Emotional Well-Being
For many, the experience of sustained stress produces a cascade of emotional responses. Cortisol is deeply involved in this process; its effects on the brain can make one more prone to anxiety and stress, which in turn further stimulates its secretion. Over time, high cortisol levels can disrupt the balance of other neurotransmitters, setting the stage for mood disorders.
Numerous studies have linked high cortisol with the development of depression. The hormone’s chronic presence can impair neural connectivity and reduce the production of serotonin and dopamine—chemicals that play crucial roles in mood regulation and happiness. This biochemical shift often results in persistent feelings of sadness, hopelessness, and overall emotional instability.
Impact on Cognitive Function and Memory
Elevated cortisol levels are also associated with impairments in cognitive function. The hippocampus, a region of the brain pivotal for forming and retrieving memories, is particularly sensitive to cortisol. Prolonged exposure to high levels of the hormone can lead to shrinkage in this region, leading to difficulties with learning and memory retention. This effect not only impacts academic and professional performance but also diminishes the overall quality of life.
In everyday scenarios, these cognitive changes may manifest as trouble focusing during important tasks or forgetting details that would typically be managed effortlessly. Such changes, when combined with other stress-related symptoms, contribute to a decline in both work efficiency and personal productivity.
The Vicious Cycle of Cortisol and Mental Health
In many cases, the mental health consequences of elevated cortisol levels create a self-perpetuating cycle. Chronic stress leads to increased cortisol production, which in turn exacerbates anxiety and depression. This chronic state then reinforces the stress response, further driving cortisol production. Breaking this cycle is often a multifaceted process that may require professional guidance, lifestyle changes, and, in some instances, medical intervention.
Addressing mental health in the context of high cortisol involves both psychological therapies and physical health interventions. Cognitive-behavioral therapy (CBT), mindfulness practices, and stress reduction techniques have shown promise in not only reducing perceived stress but also lowering cortisol levels. These strategies, when combined with appropriate medical care, can provide a robust framework for managing both the mental and physical impacts of prolonged cortisol elevation.
Diagnostic Approaches and Medical Evaluation
Determining whether high cortisol is at the root of one’s symptoms requires a careful and systematic diagnostic approach. Healthcare professionals generally rely on a combination of clinical assessment and laboratory tests to evaluate cortisol levels.
Laboratory Testing and Sampling Techniques
Several diagnostic tests are available to measure cortisol levels accurately. One of the most common methods is the saliva cortisol test, which is non-invasive and offers a practical way to monitor cortisol levels throughout the day. Since cortisol follows a diurnal rhythm—typically peaking in the morning and declining throughout the day—multiple samples may be collected to understand the full pattern of secretion. Blood and urine tests are also commonly employed, each with its own advantages and limitations regarding timing and accuracy.
Healthcare providers often recommend a 24-hour urine collection to assess cortisol levels comprehensively. This method captures the total cortisol output over the course of a day, providing valuable insights into whether the body is maintaining a normal rhythm or if there are anomalies that suggest an underlying issue.
Evaluating Underlying Conditions
When high cortisol levels are identified, further diagnostic procedures are often necessary to ascertain the cause. Imaging studies, such as CT scans or MRIs of the adrenal glands, may be indicated if there is a suspicion of an adrenal tumor or hyperplasia. In cases where Cushing’s syndrome is suspected, additional endocrine testing may be required to confirm the diagnosis and exclude other potential sources of hormonal imbalance.
The diagnostic process is as much about ruling out other conditions as it is about confirming high cortisol levels. Because the symptoms of elevated cortisol can mimic those of other disorders—ranging from thyroid dysfunction to metabolic syndrome—a thorough and multifaceted approach is essential for an accurate diagnosis.
The Role of the Healthcare Provider
A key aspect of diagnosing and managing high cortisol levels is the relationship between the patient and their healthcare provider. Open communication about lifestyle, stress levels, sleep habits, and diet can all provide important clues that contribute to a holistic assessment of the patient’s health. By taking into account both quantitative measures (such as lab tests) and qualitative information (such as personal experiences and symptoms), clinicians can develop a more accurate picture of the patient’s condition and tailor treatment strategies accordingly.
Early detection and intervention are crucial. By identifying the signs of elevated cortisol early, healthcare providers can implement strategies that may prevent the progression to more severe chronic conditions, safeguarding both physical and mental health.
Treatment Strategies and Lifestyle Modifications
Once high cortisol levels have been diagnosed, the next step is to develop a comprehensive treatment plan aimed at reducing the hormone’s adverse effects and restoring balance to the body’s systems. Treatment strategies tend to be multifaceted, combining medical interventions, lifestyle modifications, and sometimes psychological support to achieve a lasting improvement in health.
Medical Treatments and Therapeutic Interventions
Depending on the severity and underlying cause of elevated cortisol, healthcare providers may prescribe medications to help regulate hormone production. In cases of Cushing’s syndrome or other adrenal disorders, surgical removal of an adrenal tumor might be necessary. In other scenarios, medications such as ketoconazole may be used to inhibit cortisol synthesis.
For patients whose high cortisol levels are primarily stress-induced, the focus is on interventions that help manage stress and reduce cortisol output. In these cases, healthcare providers may suggest short-term pharmaceutical support to manage symptoms while encouraging long-term lifestyle changes.
The Importance of Diet and Nutrition
Lifestyle modifications play a critical role in managing high cortisol levels. An anti-inflammatory diet that includes plenty of fruits, vegetables, lean proteins, and whole grains can support overall hormonal balance. Reducing the intake of processed foods, sugars, and excessive caffeine or alcohol is especially important, as these foods can trigger or exacerbate stress responses that elevate cortisol.
Nutrients such as omega-3 fatty acids, magnesium, and vitamin B complex have been shown to influence stress levels and support adrenal function. Focusing on balanced meals throughout the day not only helps stabilize blood sugar levels but also contributes to reducing the body’s stress response over time.
Integrating Exercise into Daily Routines
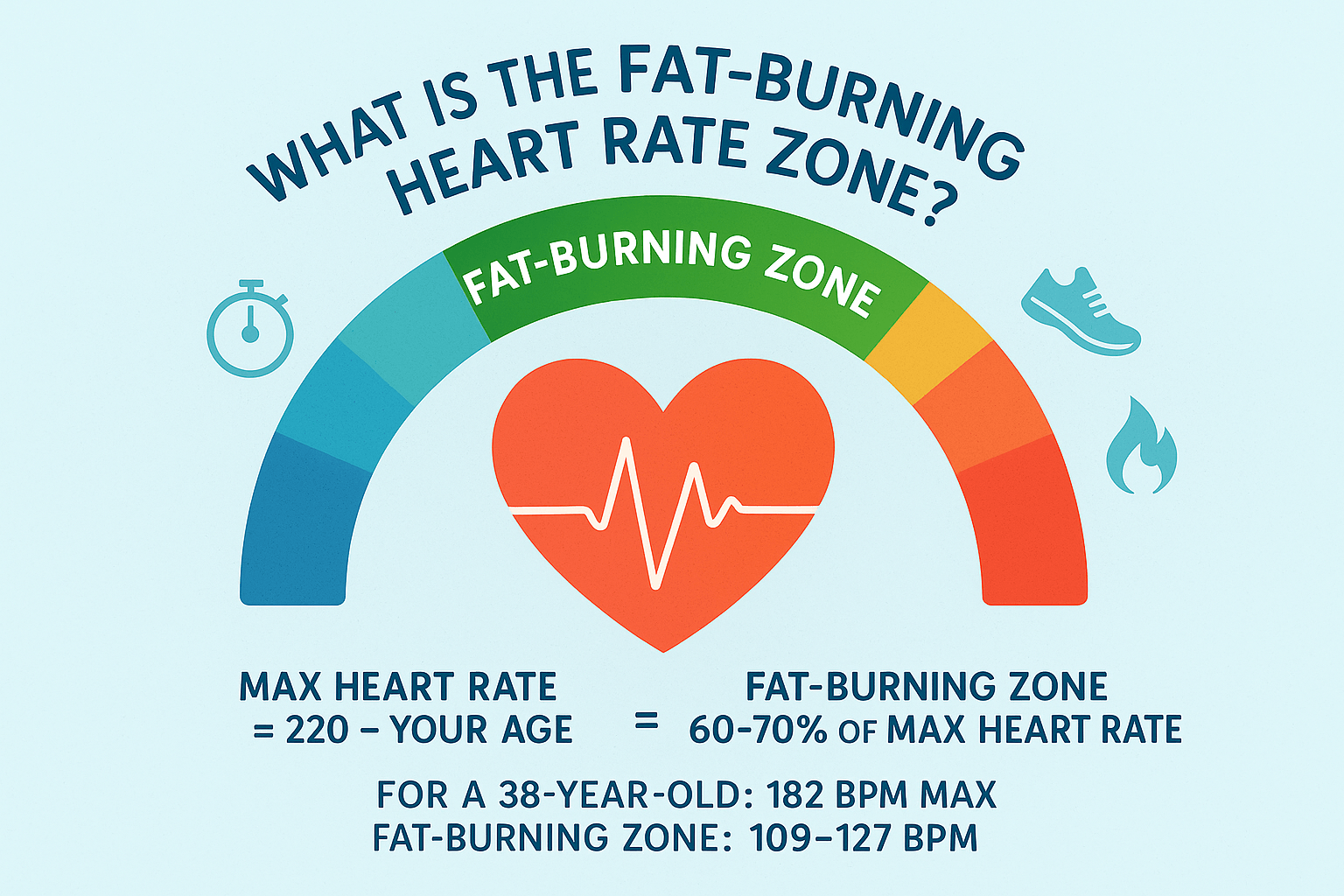
Regular physical activity is a proven method for lowering stress and consequently cortisol levels. Aerobic exercises, strength training, and activities like yoga and tai chi have all demonstrated benefits in reducing stress hormones. While excessive or overly intense exercise can sometimes raise cortisol levels, balanced, moderate activity is generally recommended as part of a healthy lifestyle.
Exercise offers dual benefits—it not only helps in reducing stress but also improves cardiovascular health, promotes better sleep, and elevates mood. Each of these benefits further contributes to lowering cortisol levels and mitigating the long-term impacts of chronic stress.
Mindfulness, Relaxation, and Stress Management
Mindfulness-based strategies and relaxation techniques are also critical components of a comprehensive treatment plan for high cortisol. Practices such as meditation, deep breathing exercises, and progressive muscle relaxation can help lower perceived stress and directly influence cortisol levels. Regular practice of these techniques encourages a calm mindset, which can significantly reduce the body’s stress response.
Therapeutic approaches like cognitive-behavioral therapy (CBT) have also been effective in helping individuals manage the psychological components of stress. By learning how to restructure negative thought patterns and reduce anxiety, patients may experience a corresponding drop in cortisol production.
Emphasizing Rest and Recovery
Quality sleep is another cornerstone of cortisol regulation. Establishing a consistent sleep routine—with regular bedtimes, a conducive sleep environment, and minimal electronic distractions—is essential for allowing the body to reset its hormonal balance each night. Sleep not only supports physical recovery but also plays a vital role in mental health, offering respite from the day's accumulated stress.
Healthcare professionals routinely advise that reducing stress and improving sleep quality are intertwined processes. When individuals feel well-rested, they are better equipped to handle stress, further promoting balanced cortisol levels and enhanced overall health.
The Broader Impacts of High Cortisol on Health and Quality of Life
Persistently elevated cortisol levels have far-reaching effects beyond the immediate symptoms. The hormone’s influence extends to almost every system in the body, affecting quality of life in both direct and subtle ways.
Implications for Metabolic Health
One of the most concerning impacts of high cortisol is its effect on metabolism. Elevated cortisol can impair insulin sensitivity, leading to an increased risk of developing type 2 diabetes and other metabolic disorders. Additionally, the hormone’s role in promoting central fat accumulation heightens the risk for cardiovascular disease. This intricate interplay between cortisol and metabolism emphasizes the importance of hormone regulation as a cornerstone of preventive healthcare.
The Cardiovascular Consequence
High cortisol levels contribute to increased blood pressure, placing extra strain on the heart and vascular system. Over time, this sustained pressure can lead to chronic hypertension, thereby increasing the risk of heart attacks, stroke, and other vascular conditions. The link between stress, cortisol, and cardiovascular health has sparked widespread interest in stress management as a means of preventing these serious conditions.
Musculoskeletal and Immune System Effects
Beyond its metabolic and cardiovascular implications, elevated cortisol has notable effects on the musculoskeletal system. High cortisol levels can lead to muscle wasting and bone density loss, making individuals more susceptible to injuries and fractures as they age. Additionally, cortisol has an immunosuppressive effect—while this can be beneficial in controlling inflammation during acute stress, prolonged suppression can weaken immune defenses, leading to an increased risk of infections and slower recovery from illnesses.
Quality of Life and Psychological Well-Being
When cortisol levels remain chronically high, the cumulative effects on quality of life become significant. Fatigue, cognitive decline, and mood disturbances not only interfere with daily routines but also impact work performance, social interactions, and overall satisfaction with life. The psychological burden of continually feeling “stressed” or “burned out” can create further emotional distress, creating a feedback loop that reinforces hormonal imbalance.
Ensuring that the broader consequences of high cortisol are addressed as part of a holistic approach is essential for long-term health. This means that prevention, early diagnosis, and comprehensive treatment are critical for mitigating not only the physiological effects of cortisol but also the overall impact on an individual’s life.
Preventative Measures and Long-Term Strategies
Given the extensive impact of high cortisol levels on overall health, prevention emerges as a key component of a wellness strategy. By adopting long-term changes and healthy habits, individuals can reduce their risk of developing cortisol-related complications while promoting a balanced internal environment.
Building a Resilient Lifestyle
Developing resilience to stress starts with conscious lifestyle choices. Prioritizing regular physical activity, consistent sleep patterns, and a balanced diet can significantly contribute to maintaining a stable cortisol rhythm. Many experts advocate for an integrative approach, where mind and body practices are combined to enhance overall resilience. Engaging in activities that promote relaxation—whether it be through hobbies, social connections, or structured meditation sessions—helps create a buffer against daily stressors.
Integrating Professional Guidance
For individuals experiencing persistent symptoms of high cortisol, seeking professional guidance is an important step. Medical professionals can offer individualized assessments and recommend tailored interventions. In some cases, working with a nutritionist, a mental health counselor, and an endocrinologist may be necessary to address all aspects of cortisol dysregulation comprehensively. Early intervention not only prevents further complications but also provides support and education to empower patients in managing their stress.
Education and Public Health Outreach
Raising public awareness about the dangers of chronically elevated cortisol is vital. By understanding both the causes and the symptoms, communities can take proactive measures to reduce stress and its harmful effects. Educational campaigns, workplace wellness programs, and community health initiatives are all critical avenues for spreading information. The goal is to help individuals recognize the signs of high cortisol early and adopt lifestyle changes that can mitigate its impact.
Moreover, public health initiatives that promote regular health screenings and stress management workshops can empower people to take charge of their well-being. By investing in education and access to resources, communities can foster a more informed populace that understands the deep interconnections between stress, hormone regulation, and overall health.
The Future of Cortisol Management Research
As research continues to delve into the complexities of cortisol regulation, emerging therapies and diagnostic tools hold promise for more effective management of high cortisol levels. Innovations in endocrinology and stress management provide hope for targeted interventions that not only reduce cortisol production but also reverse some of its long-term detrimental effects. Keeping abreast of these developments through regular consultations with healthcare providers is essential for anyone interested in managing their stress response effectively.
Ongoing studies are continually refining our understanding of how cortisol interacts with other bodily systems, paving the way for more sophisticated treatment options. This evolving body of knowledge highlights the importance of combining current scientific insights with personal health strategies to achieve optimal well-being.
Integrating a Holistic Approach to Stress Management
Ultimately, addressing high cortisol levels requires a holistic approach that integrates physical health, mental well-being, and environmental factors. This comprehensive strategy involves not just treating the symptoms, but also uncovering and addressing the root causes of stress.
Lifestyle Coaching and Behavioral Change
Working with a health coach or therapist who specializes in stress management can be incredibly beneficial. These professionals help individuals identify sources of stress, develop practical coping strategies, and implement small yet sustainable lifestyle adjustments. Such an approach emphasizes long-term change rather than quick fixes, creating a solid foundation for improved health.
Mind-Body Interventions
Mind-body techniques such as mindfulness meditation, yoga, and tai chi offer powerful tools for reducing cortisol levels. These practices have been scientifically shown to lower stress hormone levels through a combination of physical movement, breath control, and focused attention. Regular engagement in these activities not only helps lower immediate stress but also builds lasting mental resilience and physical balance.
Community and Social Support
The role of community cannot be underestimated when it comes to managing stress and cortisol levels. Strong social support networks provide emotional resources that help reduce the perception of stress. Participating in group activities, whether fitness classes, discussion groups, or creative endeavors, can provide a sense of belonging and reduce the isolation that often exacerbates stress.
Communities that foster supportive environments contribute to overall wellness by ensuring that individuals have access to resources and encouragement when navigating life’s challenges. These collective efforts highlight the interconnectedness of personal health and public health initiatives.
Navigating the Path Forward: Practical Takeaways
With a clearer understanding of both the causes and the warning signs of elevated cortisol, individuals can take proactive steps to regain control over their health. Here are some practical takeaways to consider:
For those experiencing persistent signs of high cortisol—such as unexplained weight gain, chronic fatigue, and mood disturbances—it is advisable to seek medical advice. Early detection through proper testing and diagnosis can make a significant difference in treatment outcomes. Addressing these symptoms quickly may prevent further complications, such as metabolic or cardiovascular issues.
Additionally, integrating daily practices that encourage stress reduction can help maintain healthy cortisol levels over time. Whether through regular exercise, a balanced diet, mindfulness practices, or simply setting aside time for relaxation, each of these steps contributes to a stronger, more resilient body. The journey to managing cortisol effectively is gradual, requiring patience and a commitment to lifestyle changes, but the long-term rewards in improved health and well-being are substantial.
Finally, it is important for public health messaging to underline the interconnectedness of physical and mental health. By raising awareness about the complexities of cortisol regulation, communities can empower individuals to take active steps toward a healthier lifestyle. Education, combined with accessible resources and supportive healthcare environments, creates the ideal conditions for managing stress and preventing chronic health conditions associated with high cortisol.
Conclusion: Embracing Balance and Resilience in a Stressful World
In an increasingly fast-paced and demanding world, understanding the role of cortisol is more important than ever. Elevated cortisol levels are not simply a byproduct of a busy lifestyle—they are a critical indicator of how well the body is managing the relentless pressures of modern living. By recognizing the triggers and symptoms of high cortisol, individuals can intervene before the hormone’s harmful effects take root.
This comprehensive exploration has shed light on the multifaceted nature of cortisol regulation. From the biochemical pathways of the HPA axis to the clinical manifestations of cortisol excess, each aspect of this topic underscores the importance of a balanced internal environment for long-term health. The journey toward managing stress and maintaining healthy cortisol levels is one that involves attention to diet, exercise, sleep, and mental health—the pillars of a healthy life.
In closing, embracing a holistic approach that includes regular medical evaluations, lifestyle modifications, and supportive community environments will go a long way in preventing the adverse effects of high cortisol. Whether you are seeking to understand the physiological mechanisms or looking for practical advice to manage daily stress, the key takeaway is clear: Knowledge, balanced living, and proactive management are your best allies in preserving health and achieving resilience in the face of life’s challenges.
Through a collaborative effort between individuals, healthcare professionals, and public health initiatives, we can transform our collective understanding of stress and hormonal balance into actionable solutions for a healthier, more vibrant future.