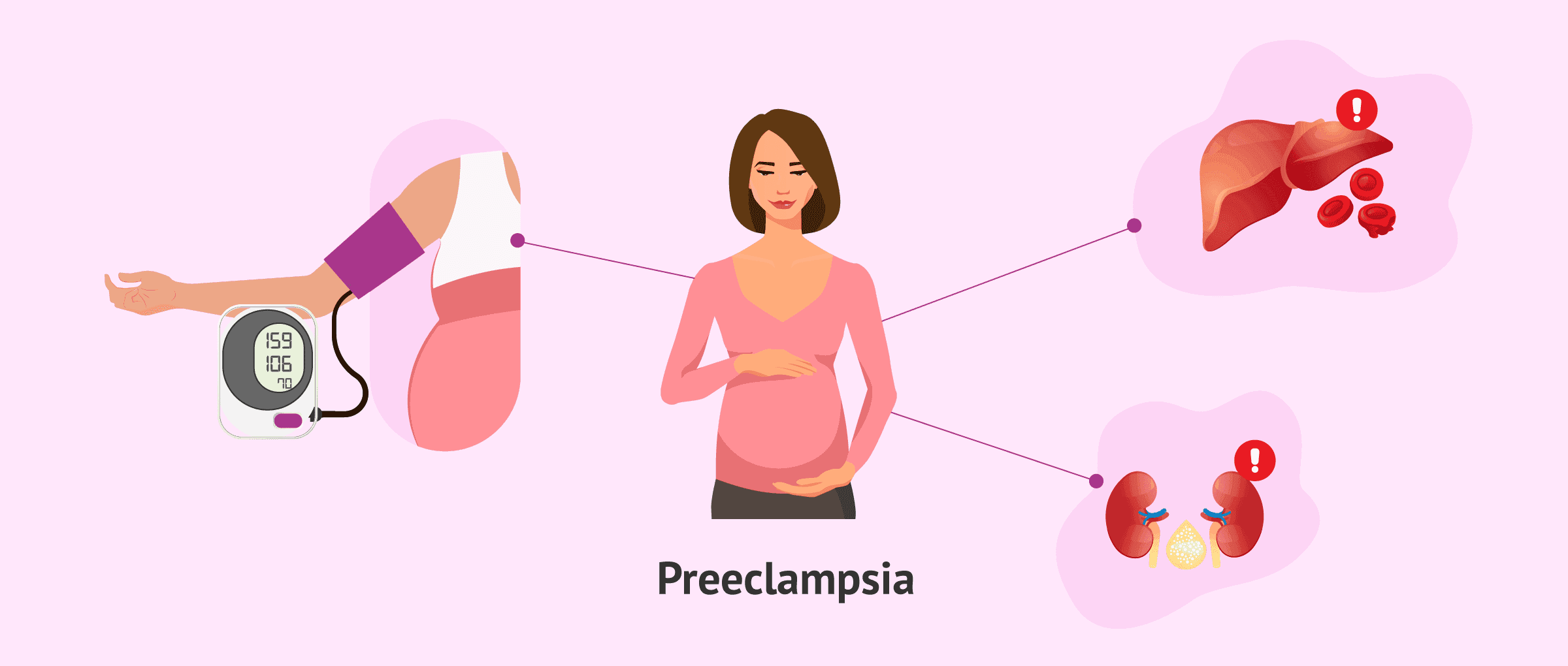
Preeclampsia is a serious pregnancy complication characterized by high blood pressure and signs of damage to other organ systems—most often the kidneys or liver. When it progresses to a severe form, both maternal and fetal health can be at significant risk. This article outlines definitions, monitoring protocols, therapeutic strategies before and after delivery, and criteria for ending the pregnancy in cases of severe preeclampsia.
1. What Is Severe Preeclampsia?
A diagnosis of severe preeclampsia is made when pregnant individuals with preeclampsia meet at least one of the following:
-
Severe hypertension:
-
Systolic ≥ 160 mmHg and/or diastolic ≥ 110 mmHg
-
-
Renal impairment:
-
Oliguria (< 500 mL urine output over 24 hours)
-
Serum creatinine > 135 µmol/L
-
-
Pulmonary or hematologic involvement:
-
Acute pulmonary edema (OAP)
-
HELLP syndrome (Hemolysis, Elevated Liver enzymes, Low Platelets < 100 × 10⁹/L)
-
-
Neurologic signs:
-
Eclampsia (seizures)
-
Severe headaches, visual disturbances, or hyperactive reflexes
-
2. In-Hospital Monitoring
2.1 Clinical Surveillance
-
Blood pressure: automated readings every 30 minutes
-
Urine output: measured hourly
-
Neurological checks: level of consciousness, reflexes (deep tendon reflexes), severe headache or visual changes
-
Respiratory status: watch for shortness of breath with pulse oximetry
-
Other warning signs: epigastric pain, worsening edema
2.2 Laboratory Monitoring
-
Every 24 hours:
-
Liver function: bilirubin, haptoglobin, LDH, CPK
-
Kidney function: serum creatinine, electrolytes; 24-hour urine protein (albuminuria)
-
Uric acid
-
-
Every 8–12 hours (in very severe cases):
-
Liver enzymes (ASAT, ALAT)
-
Complete blood count with platelet count and schistocyte screen
-
Full coagulation profile
-
2.3 Imaging
-
Maternal liver ultrasound if HELLP syndrome is suspected
-
Brain CT or MRI if neurological symptoms develop
-
Fetal monitoring: daily cardiotocography (CTG), ultrasound assessments, Doppler studies
3. Antenatal Therapeutic Strategies
3.1 Blood Pressure Control
-
First-line: Intravenous nicardipine bolus (0.5–1 mg) to target mean arterial pressure (MAP) < 140 mmHg or systolic < 160 mmHg, followed by continuous infusion (in glucose solution).
-
Add labetalol early if reflex tachycardia occurs or if more than 2 mg/h nicardipine is needed—combination therapy often provides better control.
-
Beta-blocker contraindications: consider intravenous clonidine.
3.2 Fluid Management
-
Use cautiously—avoid routine aggressive fluid loading.
-
If urine output < 600 mL in 6 hours: give 500–750 mL crystalloid (or 250–500 mL hydroxyethyl starch) over 1 hour. May repeat once, adding 20–40 mg IV furosemide if oliguria persists.
-
During prolonged fasting: maintain basal hydration and glucose with up to 1.5 L of 5% dextrose plus electrolytes.
3.3 HELLP Syndrome Management
-
Platelet transfusion if platelets < 50 × 10⁹/L before invasive procedures or delivery
-
Fresh frozen plasma if prothrombin time < 40% with planned invasive intervention or active bleeding
-
Corticosteroids (e.g., betamethasone 12 mg daily for 48 hours) may improve platelet count and liver enzymes, although not universally recommended
3.4 Eclampsia Management
-
Stop seizures: IV benzodiazepines (e.g., midazolam or clonazepam)
-
Oxygen therapy immediately
-
Magnesium sulfate regimen: 4 g IV over 20 minutes, then 1 g/h infusion for ~48 hours; monitor reflexes, respiratory rate, and mental status. Treat overdose with slow IV calcium gluconate (1 g).
-
Airway protection: intubate if Glasgow Coma Scale < 9, using thiopental and succinylcholine
-
Correct coagulopathy urgently to reduce risk of intracerebral bleeding, especially if delivery is imminent
-
Hypertension control with nicardipine plus labetalol, particularly if neuroimaging shows abnormalities
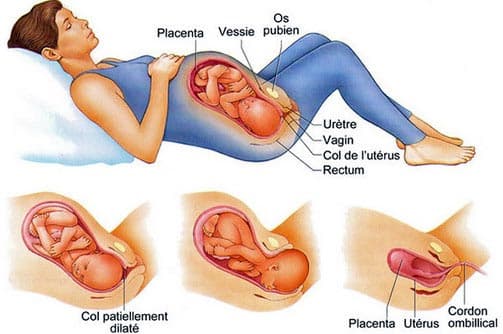
4. When to Deliver: Criteria for Pregnancy Termination
| Gestational Age | Indication |
|---|---|
| Before 24 weeks | Consider medical termination (due to very high maternal risk) |
| After 34 weeks | Delivery is generally indicated |
| Between 24–34 weeks | Decisions based on maternal (uncontrolled hypertension, HELLP progression, renal failure, neurological signs, pulmonary edema) and/or fetal distress; give corticosteroids for fetal lung maturity if time allows |
5. Postpartum Care
-
Risk period: complications may persist for at least 72 hours after delivery
-
Fluid balance: restrict intake and consider diuretics (20–40 mg furosemide) if persistent edema
-
Blood pressure: monitor closely; antihypertensives IV for first 24 hours (nicardipine 1–3 mg/h, labetalol 5–15 mg/h), then switch to oral agents
-
If breastfeeding: prefer α-methyldopa (1,000–1,500 mg/day), nicardipine, or labetalol
-
For severe hypertension: stop breastfeeding to allow use of atenolol or an ACE inhibitor
-
-
HELLP syndrome evolving postpartum: IV dexamethasone 12 mg every 12 hours until platelets > 100 × 10⁹/L, then taper
-
Thromboembolism prevention: in severe cases or heavy proteinuria, use high‐dose prophylactic low‐molecular‐weight heparin for 5 weeks once platelets are stable > 100 × 10⁹/L, along with graduated compression stockings
Conclusion
Severe preeclampsia demands vigilant clinical and laboratory monitoring, judicious use of antihypertensives and fluids, and timely decisions regarding delivery. Multidisciplinary care—obstetricians, intensivists, nephrologists, and neonatologists—ensures the best possible outcomes for both mother and baby.